Friday 26 February 2021
Lupine Publishers: Lupine Publishers | Comparative Analysis of Develo...
Lupine Publishers | Approaches to Pain Management: A Review
Lupine Publishers | LOJ Pharmacology & Clinical Research
Abstract
Pain mismanagement is associated with low recovery, high morbidity, increase hospital stay, decrease patient satisfaction, high costs of admission and adverse drug reactions due to inappropriate analgesic prescriptions. Therefore, optimal pain management is of utmost importance in promoting recovery and improving quality of life. This review describes the pharmacological and nonpharmacological approaches to the management of pain.
Keywords: Pain; Pharmacological; Non-Pharmacological; Management; Analgesics
Introduction
Pain is an unpleasant emotional situation which causes reduction in living quality and functional situation of the patients linked with increase in the fatigue levels resulting in impairments of daily life activities in working capacity and social interactions [1]. There are two types of pains: nociceptive and neuropathic pain. Nociceptive and neuropathic pains can either be acute or chronic; however, neuropathic pains are the major contributors to most chronic pains. Nociceptive pains arise from damaged tissues and wounds such as compound fracture, burns, bruises, and inflammatory disorders are typically nociceptive [2].
Pharmacological approach to the management of pain
The management of pain requires the management of the whole patient, rather than the irrational prescription of analgesic resulting to abuse of this important class of drugs without providing adequate relief of pain. The prescription of analgesic is governed by the severity of pain, the individual needs and the circumstances of the patient [3]. Pain killers (Analgesics) currently represent the mainstay of pain management, with an array of drugs available, aspirin, acetaminophen, non-steroidal anti-inflammatory drugs (NSAIDs), mixed agonist and antagonists and narcotic analgesics [4].
Non-pharmacological approach to pain management
Pain is the commonest symptom that takes patients to doctors, but the complaint does not mean that an analgesic is needed. Although drug therapy is the mainstay of pain treatment, it is not all pains that are needed to be relieved by drugs [5]. Simple measures can be used to control some types of pain. [1]. The nonpharmacological therapy of pain management is considered to help the standard pharmacological treatment in pain management. This management aims to treat the affective, cognitive, behavioral and socio-cultural dimensions of the pain. Non-pharmacological methods can be used to control some types of pain and they are invasive methods and non-invasive methods [4].
Conclusion
Optimal pain management is the right of all patients and the responsibility of all health professionals, therefore health professionals managing individuals with pain must understand the anatomy and pathophysiology of the various conditions affecting the human body as well as the mechanism and pharmacology to support the various treatment strategies. Health professionals must combine both pharmacologic and non-pharmacological methods for effective management of pain and provision of comfortable and productive life.
https://lupinepublishers.com/pharmacology-clinical-research-journal/pdf/LOJPCR.MS.ID.000132.pdf
https://lupinepublishers.com/pharmacology-clinical-research-journal/fulltext/approaches-to-pain-management-a-review.ID.000132.php
For more Lupine Publishers Open Access Journals Please visit our website: https://lupinepublishersgroup.com/
For more Pharmacology & Clinical Research Please Click
Here: https://lupinepublishers.com/pharmacology-clinical-research-journal/
To Know more Open Access Publishers Click on Lupine Publishers
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online
Wednesday 24 February 2021
Lupine Publishers: Lupine Publishers | Cerebral Autosomal Dominant Ar...
Saturday 20 February 2021
Lupine Publishers: Lupine Publishers | Cerebral Autosomal Dominant Ar...
Friday 19 February 2021
Lupine Publishers | A De Novo Mutation in TSC2 Gene is Associated with Tuberous Sclerosis Complex (TSC): A Case Report
Lupine Publishers | LOJ Pharmacology & Clinical Research
Abstract
Tuberous sclerosis, also known as tuberous sclerosis complex (TSC), is an autosomal dominant multisystem disorder characterized by hamartomas in multiple organ systems including brain, skin, heart, kidneys, and lung. These changes can result in epilepsy, learning difficulties, behavioral problems, renal failure, and other complications [1,2]. The affected genes are TSC1 and TSC2, encoding hamartin and tuberin respectively. The hamartin tuberin complex inhibits the mammalian target of rapamycin (mTOR) pathway, which controls cell growth and proliferation [2]. In this case, we report a 21-year-old Chinese female patient with TSC due to a de-nove mutation c.1806C>G (p. Tyr602Ter) in TSC2 gene [3]. This is likely to be the first report of this mutation in Chinese population. This mutation was evaluated as a pathogenic mutation based on the standards and guidelines of ACMG (American College of Medical Genetics and Genomics).
Keywords: Chinese; Epilepsy; Tuberous sclerosis complex (TSC); Tuberous sclerosis-1 (TSC1); Tuberous sclerosis-2 (TSC2); de novo mutation; ACMG
Introduction
TSC (tuberous sclerosis complex) is an autosomal dominant multi system disorder characterized by hamartomas in multiple organ systems. The genes which are related to TSC include two tumor-suppressor genes called TSC1 and TSC2. The TSC1 and TSC2 encoding hamartin and tuberin respectively. The hamartin tuberin complex inhibits the mammalian target of rapamycin (mTOR) pathway, which controls cell growth and proliferation [2]. Approximately 10 to 30% of cases of TSC are due to mutations in the TSC1 gene, the frequency of cases due to mutations in the TSC2 gene is consistently higher. TSC2 mutations are associated with more severe diseases [1]. The mutation of the gene TSC2 (c.1806C>G; p. Tyr602Ter) we detected does not exist in either Chinese population or any other populations. It has been identified as a pathogenic mutation in Clinvar database based on the hypotheses [4]. However, as of today, no detailed clinical study data or published research articles are found to support these hypotheses. It is likely to be the first clinical report of this mutation in the Chinese population.
Case Report
A 21-year-old female patient who was born with no family history of seizures or other types of neurological disease has experienced Tuberous sclerosis complex (TSC) since she was 13-year-old. The patient experienced seizures seven to eight times per month. Most of the seizures occurred during the daytime and were presented as tonic-clonic seizures which lasted approximately 2 minutes in length. There was no obvious symptom prior to the seizures. But whenever the seizures occurred, the patient would experience severe fatigue over the whole body. Besides seizures, there were several other clinical features including mental retardation, a sebaceous adenoma and a brown-pigment patch on her forehead, many depigmentation spots of different sizes on her neck, chest, back and limbs. The clinical diagnosis of her seizures was epilepsy, but the exact cause of her seizures was not found. However, according to MRI scan which showed a nodular sclerosis at the parenchyma of her brain and various other diagnoses, tuberous sclerosis complex (TSC) was highly likely to be the cause of her epilepsy. As displayed in Figure 1A, the patient’s Electroencephalography (EEG) showed frequent slow complex waves in the left anterior temporal area and the middle temporal area. Antiepileptic drugs of Carbamazepine, Zolosamide, and Everolimus were prescribed, and the improvement of the syndromes of the patient was observed after one year, as the patient experienced less seizures (Figure 1B).
In order to identify the causes of her disease, we conducted a Whole Exome Sequencing (WES) based on Next-generation sequencing. A heterozygous nonsense mutation c.1806C>G (p. Tyr602Ter) in TSC2 gene (reference transcript, NM_000548) was discovered in the patient. This mutation rarely occurs among either Chinese or any other ethnic groups, as it was not reported in mutation frequency databases including 1000 Genomes Database and genome AD database. This variant was further confirmed by Sanger Sequencing and was not detected in either of her healthy parents or her healthy younger brother, which indicated that this variant was a de novo mutation (Figure 2). This variant was evaluated as pathogenic mutation based on the standards and guidelines of ACMG. So far, this has been the first report of the mutation in Chinese population.
(red rectangles).
Discussion
In this case, we evaluated WES data from
253 Chinese patients with epilepsy and identified a de-nove heterozygous
nonsense mutation in TSC2 gene (c.1806C>G (p. Tyr602Ter) in a 21-yearold
female patient with Tuberous sclerosis complex (TSC). Sanger Sequencing further
confirmed that it is a de novo mutation since no mutations were detected in
either of her healthy parents or younger brother. This variant was evaluated as
pathogenic mutation based on the standards and guidelines of ACMG.
The mutation of the gene TSC2 we detected (c.1806C>G (p. Tyr602Ter) has been
identified as a pathogenic mutation in Clinvar database based on the following
two hypotheses. First, the Y602X variant is not observed in large population
cohorts. Second, the mutation causes the loss of normal protein function
through either protein truncation or nonsense-mediated mRNA decay pathway [4].
However, as of today, no detailed clinical study data or published research
articles are found to support these hypotheses. Our study provided some
evidence for the cause of TSC from a genetic level, and it is likely to be the
first report of this mutation (p. Tyr602Ter) in Chinese population.
Furthermore, our identification of this denove mutation in TSC2 gene might be
helpful for advancing our understanding the role of TSC2 in TSC. The TSC2
mutations are usually detected in random cases with a frequency ranging from
75% to 80%. About 15% to 20% patients do not have identifiable mutations, which
may due to mosaicism [1,2].
Conclusion
A novel nonsense mutation in TSC2 gene (c.1806C>G (p. Tyr602Ter) was identified in a 21-year-old Chinese female patient with Tuberous sclerosis complex (TSC). This is the first report in Chinese population, which may enrich the understanding of the causes of TSC.
https://lupinepublishers.com/pharmacology-clinical-research-journal/pdf/LOJPCR.MS.ID.000130.pdf
https://lupinepublishers.com/pharmacology-clinical-research-journal/fulltext/a-de-novo-mutation-in-tsc2-gene-is-associated-with-tuberous-sclerosis-complex-(tsc)-a-case-report.ID.000130.php
For more Lupine Publishers Open Access Journals Please visit our website: https://lupinepublishersgroup.com/
For more Pharmacology & Clinical Research Please Click
Here: https://lupinepublishers.com/pharmacology-clinical-research-journal/
To Know more Open Access Publishers Click on Lupine Publishers
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online
Tuesday 16 February 2021
Lupine Publishers: Lupine Publishers | Synthesis and Characterization...
Friday 12 February 2021
Lupine Publishers: Lupine Publishers | Focusing on Food Security or T...
Lupine Publishers | Ethnobotanical Survey and Identification of Potential Interactions of Plants Used in a City in Northeastern Brazil
Lupine Publishers | LOJ Pharmacology & Clinical Research
Abstract
The study of medicinal plants is currently one of the alternative sources of allopathic medicine for therapeutic purposes. Given the high consumption of medicinal plants and the risks of indiscriminate use, the objective of the study was the identification of potential plant-drug interactions in the pharmacotherapy of the Public Health System users in a Brazilian Northeastern city, from 2015 to 2017 regarding the plant species used, as well as their therapeutic properties. An ethnobotanical study was conducted with a questionnaire. For this purpose, 46 types of plants were used by the 402 interviewees, where 297 were women, with 279 adult participants, and 269 medicinal plants used. Only 199 people out of the total interviewed used some medication, of which 55 associated the use of the drug with medicinal plants. We analyzed associations between the use of 13 plants and 27 drugs, totaling 42 potential interactions. Lemon balm was the vegetal species that presented the most common interactions among the interviewees. Thus, it was possible to conclude that medicinal plants are quite used for therapeutic purposes. However, one must be cautious about its use since they can interact with drugs, reducing or potentiating their effects.
Keywords: Empirical knowledge; Interactions; Medicinal plants
Introduction
The use of medicinal plants (MPs) has been noted since the
beginning of the civilization and this practice has been passed down
through generations, drawing popular taste and leading to their
planting in the houses, trade in free markets and popular market,
as well as their use as a medicine [1]. According to the World
Health Organization, almost 80% of the worldwide population uses
medicinal plants to treat minor health problems and for several
patients this is often the only available health resource [2]. In Brazil,
it is estimated that there are between 350,000 and 550,000 plant
species, where only 55,000 are cataloged and are distributed among
different regions of the country. However, some of these species do
not have studies about their therapeutic potential, although this is
a process that has been evolving significantly [3]. In addition, Brazil
also has a long tradition of using medicinal plants linked to popular
knowledge transmitted through generation [4].
Because of their pharmacological properties, the use of MPs has
been encouraged by health regulatory agencies in order to develop
integrative/complementary methods for resolving health problems
[5]. Besides, in 2009, the Ministry of Health made available a list of
71 medicinal plants, including the National Relation of Medicinal
Plants of Interest to the Unified Health System (RENISUS), aiming
at the development of herbal medicines and use in the Public Health
System. Brazilians are also increasingly interested in “natural” ways
to promote a healthier life. Approximately 82% of the population
uses medicinal herbal products [6]. For many patients, the use of
a single drug is not sufficient, and when two or more drugs are
prescribed, the desired benefit is not always achieved, since they
may interact negatively, increasing or reducing the therapeutic
effect or the toxic effect of one or the other [7]. It should be
noted that these interactions do not reduce to the universe of the
synthesized chemical substances, but they can occur between those
present in plants used in the form of teas, homemade syrups and
phytotherapics [8]. Thus, this study aims to evaluate the use of
medicinal plants by patients from a community in the Northeast of
Brazil, aiming at tracing the profile of the plant species used, as well
as its therapeutic properties and the risk of possible plant-drug
interactions.
Methods
This is an ethnobotanical study with a questionnaire interview and collection of botanical material (when necessary). It was carried out in the municipality of Lagarto, comprising an area of approximately 968,921 km² situated in the southern portion of the state of Sergipe, Northeastern region of Brazil Figure 1, 78 km away from the capital, Aracaju. It presents a semi-arid transition climate dominating most of its lands on the western part of the municipality, where a local vegetative variety can be found [9]. It has about 103,188 inhabitants, with basically half of them residing in the rural area and the other half in the urban zone [10]. This research was carried out at the Maria do Carmo Nascimento Alves Health Center located in the municipality of Lagarto-SE. This unit targets 6 micro-regions comprising different neighborhoods and accompanied by 6 different community agents. Data collection was carried out in the region comprised by the Ademar de Carvalho neighborhood, which consists of 1,282 families accompanied by home visits of community health agents, in addition to consultations with physicians and nurses of the unit (Figure 1). In order to obtain the number of users to be interviewed, the sample calculation was performed considering a tolerable error of 5% (95% confidence), where after the calculation the minimum sample size was 296, but it was possible to apply the questionnaire to 406 users. For the calculation, the following equation was used:
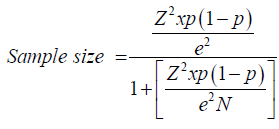
N = population size
e = margin of error (percentage in decimal format)
z = z score
It is worth mentioning that the collection was initiated after
the approval of the project by the Ethics Committee in Research
with Human Beings of the Universidade Federal de Sergipe
(protocol number 47369315.2.0000.5546). The collected material
was pressed in the field, according to [11] and identified through
specialized literature, specialist assistance and comparisons with
pre-existing specimens in the ASE Herbarium-Federal University
of Sergipe. All procedures for access to genetic patrimony and
associated traditional knowledge were carried out and the
project was registered in SISGEN (Sistema Nacional de Gestão do
Patrimônio Genético e do Conhecimento Tradicional Associado) in
accordance with Brazilian Law nº 13.123/2015 under registration
number A894E5C.
Some inclusion criteria were selected in this research: be a
user of the Maria do Carmo Nascimento Alves Health Center; be
older than 18 years and sign the TCLE - Free and Informed Consent
Form specific to this research. A brief questionnaire was applied
to the users of the Maria do Carmo Nascimento Alves Health
Center regarding their purpose, frequency, conservation, obtaining
and form of use. In addition, information was collected on the
morbidities and socio-demographic profile of the interviewees.
Some plant samples were collected in this community and
submitted to identification of the species by a botanist of the Biology
Department of the Federal University of Sergipe. Fidelity level was
calculated to quantify their importance in treating a major disease,
using the following
formula: FL = (Ip /Iu)×100
where Ip = Number of informants who suggested the use of a
species for the same main objective (therapeutic use),
(Iu) = Total number of informants who mentioned plant
species for any use [2].
The identification of potential drug-plant interactions was
carried out by means of a bibliographical survey of the plants
used, in scientific articles indexed in national and international
bases, being the bases used: Pubmed, Scielo, Lilacs, Science
direct. In addition, it was consulted through the site, the Plant-
Drug Interaction Observatory of the Faculty of Pharmacy of the
University of Coimbra. Subsequently, interactions were classified
on the pharmacodynamic or pharmacokinetic mechanism and on
the risk: mild, moderate and severe. After the questionnaires were
applied, the data were tabulated on the Microsoft Office Excel®
2007 spreadsheets, submitted to descriptive statistical analysis.
Results and Discussion
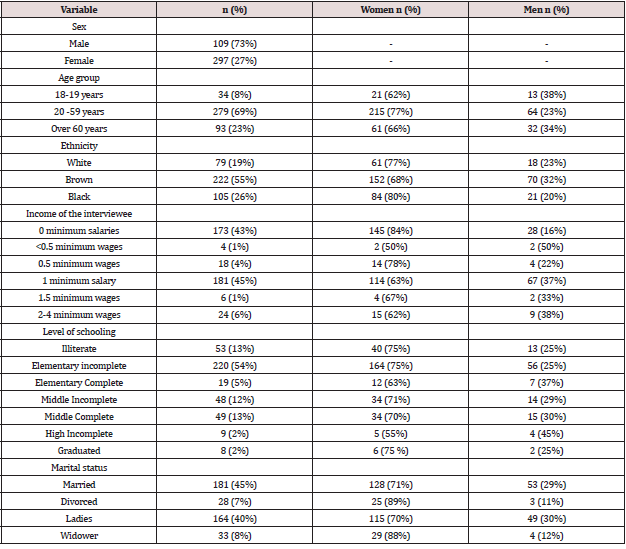
In this study, 406 people were interviewed, mostly women, all users of the Basic Health Unit in the study. The predominance of women can be justified because they are generally responsible for home and childcare, seeking knowledge about medicinal plants in order to obtain home treatments to cure or prevent diseases of family members (Lobler et al. 2013) (Table 1). Among those interviewed, the most prevalent level of schooling was the incomplete elementary school with 54%. This factor is associated with low income, which makes the use of plants a way of prevention and treatment of complications more accessible to these people.The origin of a considerable part of the plants is their own residences (Lobler et al. 2013). Socio-epidemiological profile of volunteers (Table 1) and of all the interviewees, 262 of them did not present any type of morbidity. The other 144 had morbidities such as hypertension (33%), cardiovascular problems (19%), diabetes (14%), psychological disorders (7%), respiratory problems (5%) and gastrointestinal problems (5%). In 2000, the prevalence of arterial hypertension in the world population was 25% and the estimate for the year 2025 is 29% [12].
The increase among individuals with blood pressure matches an increasing risk factor for cardiovascular diseases [13]. Of the 406 interviewees, 66% (269) stated that they used medicinal plants (MP) for therapeutic purposes, being 210 (78%) women and 59 (22%) men. Most of the interviewees use the plant species as tea. Besides, other forms of use were reported such as bath, inhalation, chewing, topical use, oral intake of the plant made as juice and syrup. The use of medicinal plants occurs over generations and the technique of preparation and conservation of these products, as well as their therapeutic purposes, are empirically passed on and generally by people who have a certain conviviality and affinity, usually relatives, friends and neighbors [14]. In fact, family members prevail with the highest number of indications, it was identified that 64% of the indications are made by one of the family (parents, grandparents, daughter-in-law and mother-in-law), 13% by self-knowledge, 8% by acquaintances, 4% by health professionals and 1% indicated by the media.
According to culture of medicinal plants was brought by the inhabitants of Brazil to be acquired by the Health System, with the purpose of providing a therapeutic alternative to the users of the system. However, for this idea to materialize, it will be necessary to implant this culture to the health professionals since the beginning of their academic formation, so that the prejudice of the use of medicinal plants for the treatment of medicinal plants can be demystified. This statement can be proven with the data obtained in this research, since only 4% of the indication of the use of medicinal plants was made by health professionals. On the other hand, 64 interviewees reported that they had already received guidance on the use of MP by health professionals, who are doctors (84%), nurses (11%), health workers (2%), nutritionists (2%) and social workers (1%). Many factors have contributed to increased use of plants as a medicinal resource, among them the high cost of industrialized medicines, the difficult access of the population to medical care, as well as the trend to use natural products. It is believed that care taken through medicinal plants is favorable to human health, provided the user has prior knowledge of its purpose, risks and benefits [15].
Participants who reported the use of medicinal plants mentioned 46 plant species (Table 2), whereby the 5 mostly used are lemon balm (213), boldo (130), holy grass (112), chamomile (58) and fennel (41). These plants are the most frequently used because they are the most popularly known and also because of their various pharmacological actions. Several studies conducted in Sergipe as well as in other northeastern regions report the use of these plants by the population. One instance is the research [15], where it is stated that the plants most frequently used by the participants were holy grass, boldo and lemon balm, corroborating with the data of this study. It made a survey of the medicinal plants used in the caatinga, where among the plants used for medicinal purposes are the ones cited in this work. Besides, it was verified that 93% of the medicinal plants reported used the leaves, 2% the stem, 3% the seed, 2% the fruit and bark and 1% the root. The predominance of leaf use can be attributed to the greater ease of collection and availability throughout the year, or also, depending on the species, due to the fact that the leaf is the organ of the plant with the highest amount of the desired metabolites [16].
Table 2: Relation between the use of the most frequent medicinal plants by the interviewees and the literature.
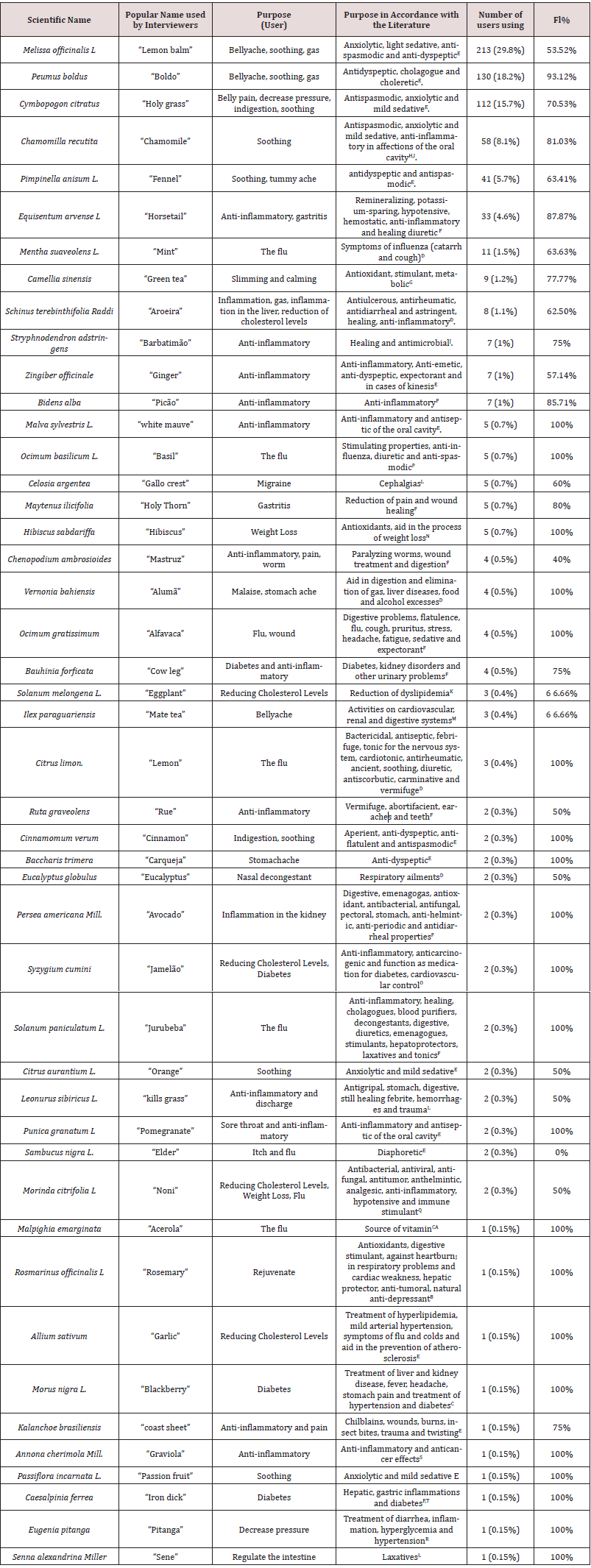
The samples of 21 plants were collected and submitted to botanical identification by a biologist. The plants were confirmed through the identification of the genus. It was not possible to identify the species because specific parts of the plants, such as roots and flowers, were needed and that was not possible at the time of collection. As it can be seen in Table 2, the popular use does not depart much from the literature, since 45 have shown use compatible with the pharmacological properties described in the literature. However, divergence or lack of scientific evidence was found. The interviewees reported that green tea Camellia sinensis has a sedative effect. However, this plant is rich in methylxanthines, such as caffeine, presenting SNC-stimulating effect [17]. Besides, this tea also has anti-inflammatory and immunomodulatory properties, which aid in the treatment of various atherosclerotic, dietetic and even carcinogenic diseases [4].
Similarly, eggplant (Solanum melongena L.) has been reported to lower cholesterol. Despite this, the literature shows that a deeper understanding of this therapeutic activity is necessary since it has not been fully elucidated [18]. Another plant that was also used with divergent purposes of the literature was the elderberry (Sambucus nigra L.) since in the literature there is still no scientific evidence to prove its action as anti-flu and to stop pruritus (Table 2) Relation between the use of the most frequent medicinal plants by the interviewees and the literature. The level of fidelity (FL) was calculated based on the number of users of a particular species of plant to treat a serious disease. The fidelity level (FL) shows the percentage of informants who use a plant species for the same disease, which is important for the total number of informants who mention the plant for any use (Table 2). Fidelity levels higher than 50% are considered as reliable for use, which was observed for most plant species, showing the importance of the use of these species in the treatment of the diseases mentioned in the study area. Peumus boldus and Equisetum sp were highly utilized plants that had the highest fidelity levels of 93.12% and 87.87% in the treatment of gastrointestinal discomforts and inflammations, respectively. Some plants had 100% fidelity level, yet these plants were little used by the interviewees, which accounts for the great index of level.
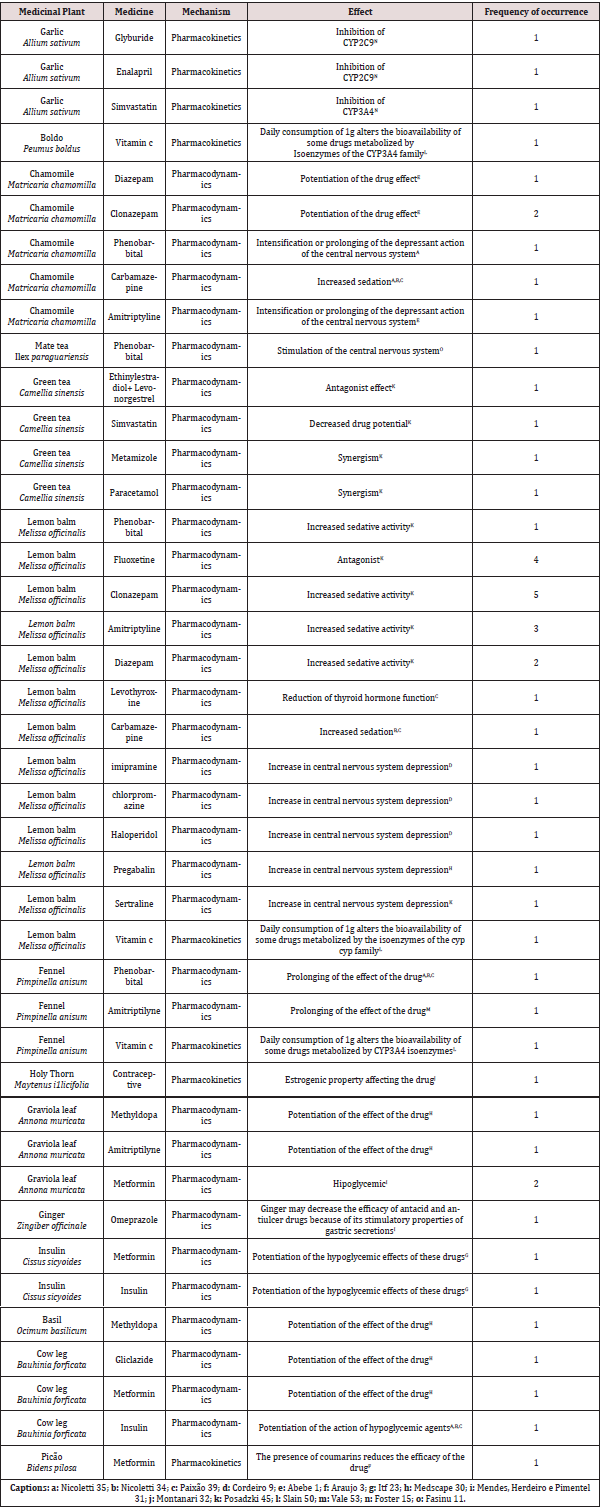
However, 55% (148) of the interviewees also use drugs and medicinal plants, presenting potential risks of interaction between MP and drugs. Therefore, we evaluated the potential interactions as shown in Table 3 and identified 42 potential interactions between MP and drugs. Of these, 90.5% (n = 38) were identified as pharmacodynamic interactions and modifications of the effector organ responses may occur, giving rise to synergistic, antagonistic, and potentiating events. Besides, 9.5% (n=4) were considered as pharmacokinetic interactions, since they are caused by a triggering drug on the absorption, distribution, biotransformation and excretion procedures of another drug, whose effect is modified (Table 3) Potential plant-drug interaction.
The lemon balm was the plant that presented the most common interactions among the interviewees since it was the most used by them. Their interaction with sedative and anxiolytic drugs such as fluoxetine, amitriptyline, clonazepam (medicines that the respondents reported use), cause increased sedative activity, and this may occur because the lemon balm exerts an additive effect when simultaneously with central nervous system depressant drugs due to their neurocognitive properties [19]. The clinical significance of drug interactions is related to their type (mechanism) and magnitude (severity). In fact, this information is useful to support the need and intensity of patient monitoring or changes in therapy to avoid possible adverse consequences [20-25], since of the 66 respondents who were advised by a health professional, 15 of these could have had potential plant-drug interactions. However, there are no data about the severity degree of plant-drug interactions, as well as the lack of a source that deals with plant-plant interactions.
In fact, plant-plant interactions are also important for their safe use. In our study, of the 406 interviewees, 67 mixed different medicinal plants in the same preparation, such as: sacred grass with lemon balm, lemongrass with chamomile, boldo with lemon balm, barberry with barbatimão, but studies on these interactions are scarce and there is no scientific evidence among these plants. However, it is worth mentioning that of the 406 participants, none reported intoxication or adverse effect related to the use of medicinal plants alone or in a mixture. In addition, 34 (8.3%) participants reported the use of phytotherapics, among whom 31 (91%) were female and 4 (9%) started use due to medical indication [26-31]. Among the phytotherapics used daily are Calmam® (Passiflora incarnata L., Propolis extract (tree resin, beeswax, flower pollen, essential oils), Vitro Naturals Noni Juice® Morinda citrifolia, Herbarium “Unha de gato”® Uncaria tomentosa, Seakalm® (Passiflora Incarnata), Calmix® (Passiflora Incarnata, Melissa officinalis, Valeriana officinalis, Erythrina verna, Cymbopogon citratus, Hypericum perforatum, Matricaria chamomilla), Valeriane® (Valeriana officinalis L.). Thus, the numbers of informants that make use of these phytotherapics are 16, 8, 2, 2, 2, 2, 2, respectively. The low consumption of phytotherapics can be strained to the little knowledge of the population since they have been recently inserted in the market because the National Policy on Integrative and Complementary Practices in the Public Health System was approved in 2006. Besides, since a great part of the interviewees is of low class, many are not able to acquire these medicines [32-38].
Conclusion
In summary, when tracing the epidemiological profile and the medicinal plants used, it was possible to conclude that the use of MPs is part of the popular culture of a city of Sergipe, a state of northeastern Brazil, and is frequently used to aid in the relief and/ or cure of symptoms or diseases, as it is also observed in other regions of the country [39-43]. It was also observed that despite advances in the production of medicines, people still use medicinal plants for therapeutic purposes, where the sociocultural aspect has a strong influence [44-47]. However, medicinal plants are not exempt from causing any harm to human health, since, in addition to toxicity, they may interact with some medicinal products [48-52], if used concomitantly with the plant, reducing or potentiating its effects, as presented in this study. In view of this, there is a need for a rational and safe use of alternative medicines and therapies, as well as the orientation of qualified health professionals and the awareness of the risks and benefits of the concomitant use of the therapies under study in order to prevent health problems [53-57].
https://lupinepublishers.com/pharmacology-clinical-research-journal/pdf/LOJPCR.MS.ID.000131.pdf
https://lupinepublishers.com/pharmacology-clinical-research-journal/fulltext/ethnobotanical-survey-and-identification-of-potential-interactions-of-plants-used-in-a-city-in-northeastern-brazil.ID.000131.php
For more Lupine Publishers Open Access Journals Please visit our website: https://lupinepublishersgroup.com/
For more Pharmacology & Clinical Research Please Click
Here: https://lupinepublishers.com/pharmacology-clinical-research-journal/
To Know more Open Access Publishers Click on Lupine Publishers
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online